Irritable bowel syndrome (IBS) is a common disorder that affects millions of people. Learn about symptoms, causes, diagnosis, treatment and more below:
What is IBS?
Irritable Bowel Syndrome (IBS) is a chronic gastrointestinal disorder that a significant number of people suffer from daily, yet it still remains misunderstood and thus difficult to treat or manage. It is estimated that around 8% of the South African population36 (approximately 4.6 million South Africans) suffer from IBS, which is defined as recurrent abdominal pain, stomach cramps and intermittent diarrhoea, on average, at least 1 day/week in the last 3 months. It is important to note that IBS is not a disease, but rather a functional disorder, meaning an abnormal function of the bowels, that results in a number of symptoms.
IBS Symptoms
Irritable Bowel Syndrome symptoms may include any combination of abdominal pain, excessive gas production, bloating, diarrhoea, and constipation. Based on the bowel movement symptoms, there are three major subtypes of IBS: the one with predominant constipation (IBS-C), diarrhoea (IBS-D), or both (IBS-M). IBS has also been strongly associated with mental health, with about 80% of IBS patients also suffering from anxiety or depression. This is due to the gut-brain axis, a direct connection between our brain and gut via the vagus nerve and neurotransmitters.
What causes IBS?
There is currently no known cause of the for IBS. However, there is increasing evidence that suggests that there may be a psychological factor, where there is ‘faulty’ communication between the brain and the intestinal tract. In some cases this disconnect results in spasms and intestinal cramping. Scientists believe that the most likely cause is nutritional and lifestyle factors. There is strong evidence that the gut microbiome dysbiosis plays a significant role in IBS. Evidence includes the overuse of antibiotics, infection, colonoscopy (intestinal prep), and postinfectious IBS, which has been confirmed in animal models. Infections that have been associated with follow-on onset of IBS include Giardiasis, Campylobacter, and specific toxin-producing strains of Escherichia coli. However, many other types of non-specific gastroenteritis have been associated with the downstream development of IBS symptoms.
The most likely cause of IBS is functional gut microbiome dysbiosis , which affects both the intestinal lining and production of neurotransmitters that influence mental health. This dysbiosiscan be established with antibiotics.
Is there a test for IBS?
IBS is diagnosed using established symptom criteria in the absence of “red flags” such as unexplained weight loss, blood in stool, or recent change in bowel habits. There is no examination or molecular test for IBS and is typically identified through a process of elimination or exclusion. Some physicians will perform a colonoscopy, which excludes other diagnoses, such as Inflammatory Bowel Disease (IBD), but does not diagnose IBS. IBS diagnosis must be obtained at a healthcare provider.
How is IBS diagnosed?
The gold standard diagnostic test, called the Rome IV criteria, is all symptoms-based. There are no blood or stool tests. The Rome criteria include two questionnaires: one to determine if a patient has IBS and which subtype, and the other one to determine the disorder severity.
IBS and Gut Health
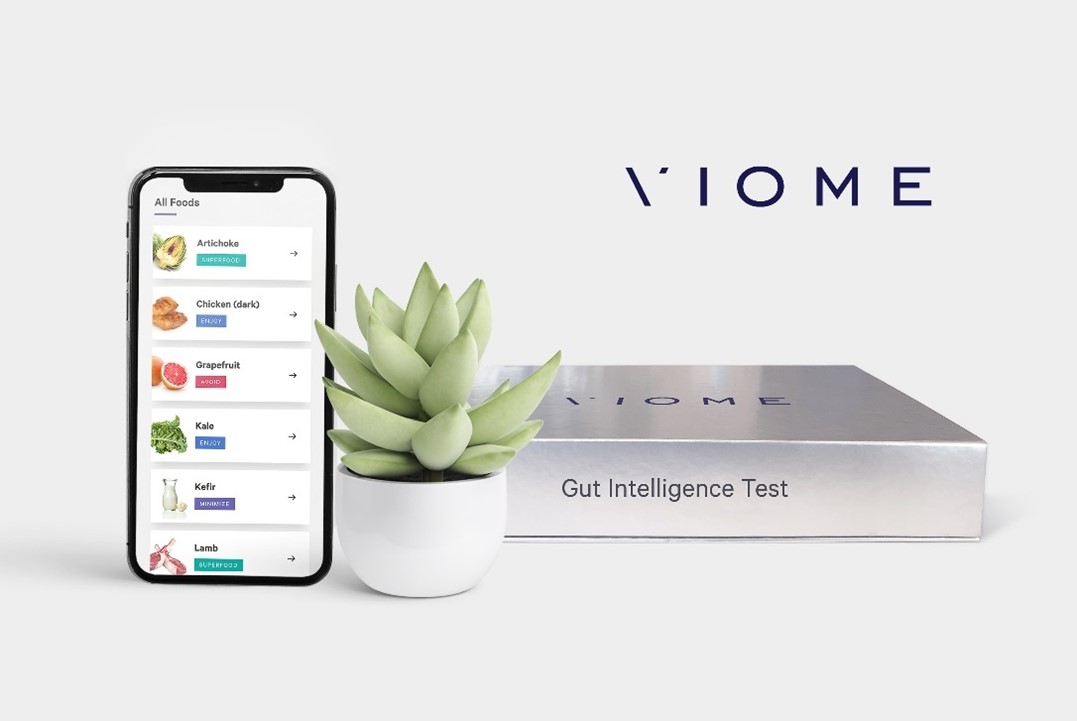
With a complex condition like IBS, knowledge is power. Since there are many causes of IBS, there is no one treatment that works for everyone. Changes in how we assess our gut health can mean more than just cleaning up your diet – it can mean the freedom to go back to living. It means feeling good about your body, traveling, socialising, and eating. It means regaining control of your life. The Viome Gut Intelligence Test can help provide people suffering from Irritable Bowel Syndrome with the nuanced information they need to finely adjust their diet, help alleviate episodes of gastrointestinal discomfort, and build up a healthy gut microbiome.
How do you treat IBS?
IBS is a chronic disorder, and there is no cure for IBS. Different approaches have been attempted as IBS therapy, all with limited success, especially long-term. Some antibiotics have shown a modest improvement in certain participants. Certain diets can relieve some symptoms of some patients. The most well-known diet that is recommended by some physicians is a low FODMAP diet. However, even when it works, most patients find it challenging to maintain. Some providers have attempted to use faecal microbiota transplants (FMTs) to treat IBS, however, there is currently no scientific evidence for the effectiveness of FMT. Cognitive Behavioural Therapy (CBT) has been shown to be at least as effective as currently available gut-targeted therapies. CBT has shown efficacy on a percentage of the IBS patient population, so this avenue should be further developed and tested.
Changes in lifestyle and diet such as regular exercise have been shown to improve some symptoms, especially constipation. Evidence also suggests that symptoms can be improved by excluding “gas-forming” foods and avoiding certain foods that "trigger" or worsen diarrhoea, bloating and gas such as cruciferous vegetables, and legumes.
Other home remedies to relieve symptoms of IBS include adding fibre to the diet, drinking plenty of water, avoiding soda, eating smaller meals, and eating more low fat and high carbohydrate foods.
Can probiotics help with IBS?
While probiotics have shown efficacy towards IBS, as with the other therapies, they work in some patients, with uncertain long-term benefits. Again, the main reason for this is that the probiotics are chosen mostly based on a scientist’s opinion and anecdotes, or a manufacturer’s favourite product. While probiotics can restore the proper balance in the gut microbiome and relieve IBS symptoms in some patients, a data-driven approach must be taken. That means that each IBS sufferer must be given a very specific combination of strains, then fed a very specific diet that will ensure effective colonization of the strains and proper functional contribution to the gut microbiome health.
Best foods to eat for IBS?
The limited success of the low FODMAP (fermentable oligo-, di-, mono-saccharides, and polyols) diets has been obtained in several clinical trials, especially when it comes to reducing the symptoms of abdominal pain and diarrhoea. However, the quality of life relative to a standard diet has been shown to be equivalent. In addition, most people have a difficult time maintaining a low FODMAP diet, and there are concerns about malnutrition during the low FODMAP diet that has been documented. Increased fibre intake has relieved symptoms of IBS, especially constipation, in some trials. However, there are no guidelines that recommend specific fibres to patients based on their microbiome. No specific foods have been identified as universally good for IBS sufferers. The reason for this is that the gut microbiome of IBS patients is very diverse compositionally. Each person needs to consume a very different diet in order for their gut microbiome to produce healthy biochemicals and stop producing disease-associated ones. Personalised diets, based on comprehensive and functional gut microbiome tests, will revolutionize the treatment of IBS, as they will truly restore the healthy functional gut microbiome for each person.
Listen to your gut.
Order Viome's Gut Intelligence kit today and have it delivered right to your home.
Only R6 900
Are there foods to avoid if you have IBS? How about coffee and alcohol?
Besides FODMAPs, there are several other foods that have been reported to have negative effects on IBS symptoms in some patients. These include high-fat foods, gluten-containing foods (which may be an overlap with FODMAPs), spicy foods, dairy, coffee, and alcohol. Because the symptoms and likely causes of IBS are so diverse, and gut microbiomes of IBS patients can vary widely, it is necessary to personalise each person’s diet in order to reduce the symptoms of IBS.
Can you cure IBS?
If the symptoms can be permanently eliminated, IBS will be effectively cured. While there are reports of curing IBS with faecal microbiota transplants (FMT), the long-lasting effects of such therapies have not been reported. Given that the symptoms change over time and that some patients experience prolonged remission, it is very likely that curative therapy is possible.
Is IBS genetic?
The contribution of genetics to IBS varies widely from study to study (from 0-57% influence), which makes it difficult to quantify. However, the majority of people who have genetic predisposition do not develop IBS, and the majority of people who have IBS do not have a genetic predisposition. Most importantly, once a person has IBS, it does not matter what their genetic predisposition is, they can heavily influence their symptoms with diet and lifestyle changes.
References
- https://theromefoundation.org/rome-iv/
- http://www.sapajournal.co.za
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6309514/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6849782/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6663289/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6984424/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4739722/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4766540/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5648751/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6508472/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7043712/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7145050/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6144954/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7282555/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2886445/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6769995/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6843426/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6036777/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7019629/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7019579/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7043591/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7146283/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7231142/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7259234/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6267171/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5056577/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6259499/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5712083/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4697992/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4505618/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6474711/
- https://www.ncbi.nlm.nih.gov/pmc/articles/PMC6914991/
- https://pubmed.ncbi.nlm.nih.gov/19031266/
- https://pubmed.ncbi.nlm.nih.gov/22457686/
- https://pubmed.ncbi.nlm.nih.gov/24047860/
- https://pubmed.ncbi.nlm.nih.gov/31885549/
- http://www.webmd.com/ibs/tc/irritable-bowel-syndrome-ibs-cause
- https://www.ncbi.nlm.nih.gov/pubmed/28573818
